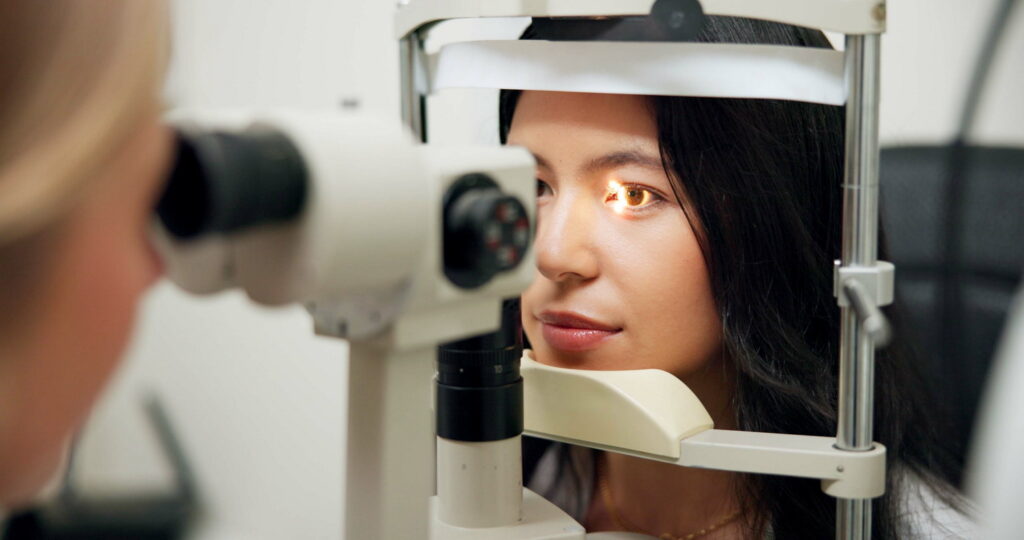
Comprehensive Retinal Services for Every Stage of Care
From diagnosis to advanced treatment and ongoing management, we offer a full spectrum of specialized care for retinal diseases to protect and preserve your vision.

We offer state of the art services treating diseases of the retina, macula, and vitreous. We focus exclusively on retinal care, ensuring that patients receive expert, subspecialty-level diagnosis and treatment.
Intravitreal Injections
Intravitreal injections are used to treat conditions like age-related macular degeneration (AMD), diabetic retinopathy, and retinal vein occlusion. This in-office procedure is quick and done with local anesthetic. The eye is cleaned with antiseptic before the injection.
Mild irritation, a scratchy sensation, or blurry vision may follow. A small red spot may appear on the white of the eye—this usually clears within two weeks. Improvement in vision can occur after a few injections, but in some cases, the goal is to stabilize the disease rather than improve vision. Possible side effects: injection site pain, floaters, lens clouding, retinal detachment, and elevated eye pressure
Common Injection Medications
Eylea (Aflibercept)
Eylea treats wet AMD by blocking VEGF, a protein that causes abnormal blood vessel growth. It helps prevent and sometimes reverse vision loss. Eylea HD is a higher dose of Eylea. It may last longer than Avastin or Lucentis.
Ozurdex
Ozurdex is a small implant that slowly releases steroid medication inside the eye. It treats diabetic macular edema, macular swelling from vein occlusions (BRVO or CRVO), and posterior uveitis. The implant dissolves naturally.
Lucentis (ranibizumab)
An anti-VEGF (vascular endothelial growth factor) drug injected into the eye to slow abnormal blood vessel growth and reduce fluid leakage in retinal diseases like wet age-related macular degeneration (AMD) and diabetic macular edema.
Vabysmo (faricimab)
A bispecific antibody that targets both VEGF-A and Ang-2 (angiopoietin-2) to improve retinal vascular stability, reduce leakage, and help preserve vision in diseases such as wet AMD and diabetic macular edema.
Avastin (bevacizumab)
Originally developed for cancer treatment, it’s often used “off-label” in eye care to block VEGF and control abnormal blood vessel growth and swelling in the retina.
Syfovre (pegcetacoplan)
A complement C3 inhibitor injected into the eye to slow the progression of geographic atrophy, an advanced form of dry AMD, by reducing overactivation of the complement immune pathway.
Izervay (avacincaptad pegol)
A complement C5 inhibitor designed to slow geographic atrophy in dry AMD by reducing complement-mediated retinal cell damage.
Laser Photocoagulation
Pneumatic Retinopexy
Pneumatic retinopexy is an in-office treatment for certain types of retinal detachment, especially in the upper retina. The eye is numbed and cleaned. A small amount of fluid is removed, and a gas bubble is injected into the eye.
The patient must maintain specific head positioning for 1–2 weeks. A few days later, laser or freezing treatment (cryotherapy) is used to seal the retinal tear. Flying and anesthesia procedures must be avoided while the gas is present.
This outpatient retina laser treatment may be used for macular edema, diabetic retinopathy, retinal vein occlusion, and retinal tears. After numbing drops, a contact lens is placed on the eye and bright laser light is applied for a few minutes. Some patients report mild discomfort. No eye patch is needed after.
Scleral Buckle
A scleral buckle is an outpatient surgery for retinal detachment. Under local or general anesthesia, a thin silicone band is placed around the white of the eye to relieve tension on the retina and help it reattach. The buckle is usually permanent and not visible. Placement of the scleral buckle causes the eye to be more near-sighted.
Vitrectomy
Vitrectomy is an outpatient surgery used to treat:
- Vitreous hemorrhage
- Retinal detachment
- Macular holes or epiretinal membranes
- Retained lens fragments (after cataract surgery)
- Diabetic retinopathy
The surgeon uses small probes (0.5mm diameter) to access and treat various parts of the eye. In some cases, larger incisions must be necessary. Laser or cryotherapy also may be used. The eye is often filled with air or gas, and much less frequently silicone oil.
After numbing the eye and cleaning it, the surgeon removes the vitreous gel through small incisions. Laser or cryotherapy may be used, and the eye is often filled with gas or silicone oil. A patch and shield are placed after surgery and removed the next day in-office. Blurry vision afterward is normal.